Introduction to Genetics
and Public Health
| This lass on genetics and public health usse a case-based approach to introduce you to contemporary issues at the intersection of public health and genetics. Our overall goal is to encourage you to recognize the genetic aspect of public health problems. Just as learning about infectious organisms two centuries ago altered public health practices, from sanitation to immunizations, new knowledge and technologies in genetics are altering and will continue to impact public health practices. Genetic information influences health and disease across the lifespan, from preconceptional genetic counseling and fortification of flours with folate to improvements in our understanding of causes of death and disability, from newborn hearing screening where over half of congenital hearing loss is genetic to recognition of the familial risk factors inherent in, for example, Alzheimer disease, cancer, coronary artery disease and stroke.
An ongoing challenge for public health personnel is to incorporate current understanding of the science of health and disease in effective and ethical public health measures. Your own understanding of the relevance of the genetic components of your family health history to your own health and your willingness to think about these complex issues for society and public health are both part of your legacy. Think genetically.
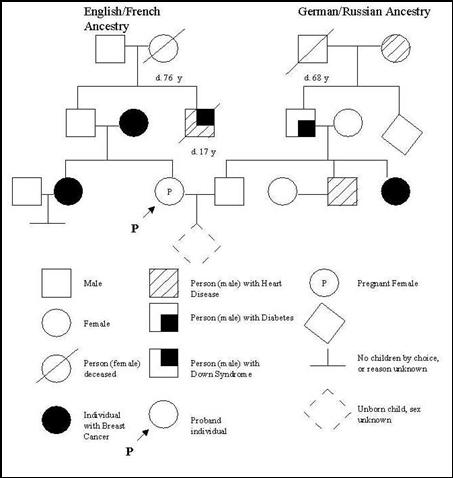
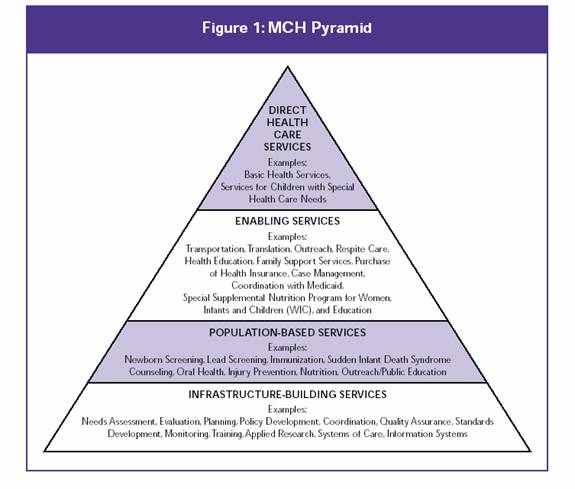
The National Coalition for Health Professional Education in Genetics (www.nchpeg.org), a coalition of more than 120 health professional organizations, and the CDC (http://www.CDC.gov/genomics/training/competencies/default.html) have developed a set of competencies in genetics for health professionals and for the public health workforce. Review these competencies and continue to reflect upon them as you go through your MPH program. The following have been identified as public health functions relevant to genetics: public health assessment; evaluation of genetic testing; development, implementation, and evaluation of population interventions; and communication and information dissemination. Critical issues include: partnerships and coordination; ethical, legal and social issues; and education and training. Genetics and Public Health in the 21st Century (Muin Khoury, Wylie Burke, Elizabeth J Thomson (eds.), New York, Oxford University Press, 2000) is a comprehensive monograph about using genetic information to improve health and human disease. The following web sites may be useful for your further study. Alliance of Genetic Support Groups (former name), now Genetic Alliance GeneReviews, GeneTests, GeneClinics Information for genetic professionals and on genetic conditions March of Dimes National Human Genome Research Institute National Coalition for Health Professional Education in Genetics Office of Genetics and Disease Prevention www.cdc.gov/genetics.default.htm OMIM, Online Mendelian Inheritance in Man Birth defects: Case 1 - Your sister has just found out at 16 weeks of pregnancy that she has a fetus with spina bifida. Describe the levels of the maternal child health pyramid that impact how this is handled. The lecture (see Birth defects and the maternal child health pyramid.ppt) will challenge you to consider how the management and prevention of birth defects with a genetic component requires the interplay and cooperation of the various levels of public health service. You are encouraged to review the following websites related to birth defects and folic acid and keep the following questions in mind. Birth defects: 1) National Center for Birth Defects and Developmental Disabilities www.cdc.gov/ncbddd/bddefault.htm 2) National Birth Defect Prevention Network Folic Acid: 1) Advocating for Folic Acid: A Guide for Health Professionals 2) National Council on Folic Acid www.folicacidinfo.org/about_us.php Maternal Child Health Pyramid:
MCH Bureau Definitions of Core Public Health Services and Key Words www.tdh.state.tx.us/mch/defs.htm
Lecture - Birth defects and the maternal child health pyramid Cancer: Case 2 - Your next-door neighbor tells you that 2 of her 4 daughters have recently been diagnosed with breast cancer. You all grew up together and are worried about the "cancer street." Describe how public health and genetic help you address risk assessment. With the completion of the Human Genome Project inherited risk factors are increasingly being identified as contributors to common chronic diseases. As clinical testing strives to keep up with research advances in genetics, public health officials are recognizing the value of family history as an important screening tool. In this part of the lecture (see The Genetic Component of a Common Disease.ppt) we use the example of cancer and cancer clusters as a paradigm for the inherited genetic contribution to common diseases, and we discuss the incorporation of genetic information into public health investigations of these diseases. After exploring these websites think about possible answers to the following questions: CDC National Center for Environmental Health (Cancer Clusters) Mid-Atlantic Cancer Genetics Network Office of Genomics and Disease Prevention at the CDC National Cancer Institute Virginia Department of Health (Cancer Registry) http://www.vdh.state.va.us/epi/cancer/index.asp
Lecture - The Genetic Component of a Common Disease Health manpower: Case 3 - You are a health planner and suddenly learn that there are no nutritionists in the state who have training in handling infants who are diagnosed on newborn screen with metabolic disease. Describe how you would address this need. The lecture (see Health manpower and newborn screening.ppt) will take you through one public health geneticist's approach to this question. You are strongly encouraged to choose one of the seven current (sickle cell and hemoglobinopathies, phenylketonuria (PKU), maple syrup urine disease (MSUD), homocystinuria, hypothyroidism, biotinidase deficiency, congenital adrenal hyperplasia (CAH)) or future medium chain acyldehydrogenase (MCAD) conditions screened for in Virginia at birth and review the following websites to answer the following questions. www.aap.org (Pediatrics 2000 Aug; 10692 pt 2)389-422. Screening the family from birth to the medical home. Newborn screening: a blueprint for the future - a call for a national agenda on state newborn screening programs) http://genes-r-us.uthscsa.edu (National Newborn Screening and Genetics Resource Center, 2000 National NBS report) www.geneticalliance.org (national coalition of genetic support groups, useful for getting information on a particular genetic condition by going to the particular condition's support group's web page) www.marchofdimes.com (look for information sheets for parents)
Lecture - Health manpower and newborn screening |
| MPH Home Page | Course Contents | Useful Web Links | Blackboard |